
Soap Note How To Write Spotless Healthcare Notes Free

How To Write Incredible Physical Therapist Soap Notes
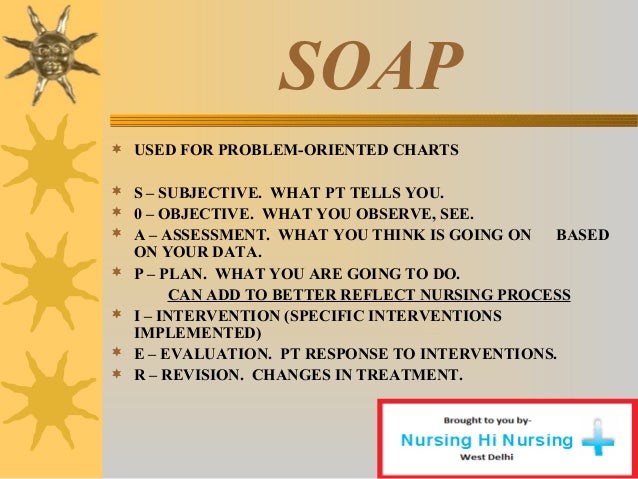
Pattern, the patient treatment records pattern which describes the collection of treatment instances for each patient within a medical group. the soap pattern for medical charts is a categorization of the patient treatment instance. 1. introduction a medical record could be thought of as a series of dated treatment instances, or encounters. each. The soap format is a common way of organizing ___ ___ in medical records. subjective, objective, assessment, plan soap is the most common format used for progress notes (or chart notes). s______ = statements about the patient's current condition and any symptoms he or she is experiencing. Pomr was the medical community’s first foray into standardizing patient records and storing it in an electronic format. since then, pomr has enabled physicians to save time as well as raise the quality of patient care and improve patient satisfaction.
Accessing Your Medical Records Online
Hospitals, pharmacies and other health care institutions maintain patients’ medical records. these institutions also issue patients copies of transaction documents for the medical expenses. it's important to record and maintain these docume. Aug 03, 2020 · some medical practices may want the fully-written soap note to be reviewed and/or approved by a higher-up, while some practices will want the soap note writer to upload the completed document to a database of medical records. or, the best plan of action may be to carry out soap in medical records the action tasks in the plan as soon as possible. Soap notes are used for admission notes, medical histories and other documents in a patient’s chart. many hospitals use electronic medical records, which often have templates that plug information into a soap note format. most healthcare clinicians including nurses, physical and occupational therapists and doctors use soap notes.
Your medical records—whether they’re all at your family doctor or scattered at different clinics around town—are yours to access. having a copy can help you save money, get better care, or just satisfy your curiosity. your medical records—w. How to write medical soap notes. in the medical worls, "soap" stands for subjective, objective, assessment and plan. the soap note soap in medical records is a daily notation of a patient's condition, progress and immediate plan for diagnosis and treatment. a well. Consumer's rights with respect to their medical records hhs hipaa home for individuals your medical records this guidance remains in effect only to the extent that it is consistent with the court’s order in ciox health, llc v. azar, no.

In the united states, you have the legal right to obtain any past medical records from any hospital or physician. retrieving old records, even those stored on microfilm, can be a simple process, depending on the hospital's policy for storin. It’s a patient’s right to view his or her medical records, receive copies of them and obtain a summary of the care he or she received. the process for doing so is straightforward. when you use the following guidelines, you can learn how to.
Struggling with your own files or those of a loved one you care for? due to interest in the covid-19 vaccines, we are experiencing an extremely high call volume. please understand that our phone lines must be clear for urgent medical care n. Soap notes are commonly found in electronic medical records (emr) and are used by providers of various backgrounds. generally, soap notes are used as a template to guide the information that physicians add to a patient's emr. Dec 19, 2017 · while there are many ways a physical therapist can document patient progress, physical therapy soap notes are the most comprehensive and structured way to go. these notes are carefully maintained within the patient’s medical records. detailed patient notes are important as they help keep communication flowing seamlessly between providers. Whether you're interested in reviewing information doctors have collected about you or you need to verify a specific component of a past treatment, it can be important to gain access to your medical records online. this guide shows you how.
Soap note: how to write spotless healthcare notes (free.
Generally speaking, a soap note is a short form organizing a patient’s personal and medical information and they are used primarily for admissions, medical history, and a few other documents in a patient’s chart. there are generally four parts to this note. In general, entities in possession of medical records are required to maintain those records for a given period. in the united kingdom, medical records are required for the lifetime of a patient and legally for as long as that complaint action can be brought. generally in the uk, any recorded information should be kept legally for 7 years, but.
Soap notes were developed by dr. lawrence weed in the 1960's at the university of vermont as part of the problem-orientated medical record (pomr). each soap note would be associated with one of the problems identified by the primary physician, and so formed only one part of the documentation process. Developed by dr/ lawrence weed in the 1960s, the soap note template methodology records vital patient medical information, to provide evidence of patient contact, and to inform a clinical reasoning process. soap notes have four main parts, designed to help improve evaluations and standardize documentation: subjective what the patient tells you.
Practicestudio is a best-of-breed electronic health records software that has successfully served medical clinics for soap in medical records more than 25 years. from the very beginning we have been committed to a complete solution that is seamlessly integrated between our practice management and medical records. Your private medical record is not as private as you may think. here are the people and organizations that can access it and how they use your data. in the united states, most people believe that health insurance portability and accountabil.
Documenting a patient assessment in the notes is something all medical students need to practice. this guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner. you might also find our other documentation guides helpful. Request patient medical records, refer a patient, or find a ctca physician. to request your patient's medical records from one of our hospitals, please call or fax one of the numbers below to start the process. to refer a patient to ctca, p. The soap note stands for subjective, objective, assessment, and plan. this note is widely used in medical industry. doctors and nurses use soap note to document and record the patient’s condition and status. the soap note is considered as the most effective and standard documentation used in the medical industry along with the progress note. Soap acronym for subjective data, objective data, assessment, soap in medical records plan, the way the progress notes are organized in problem-oriented record keeping. soap [sōp] any compound of.
Jan 27, 2021 · medical records often contain highly sensitive and private information. only specific individuals have access to your medical records. states vary in procedures and policy in regards to handing out medical records, as do individual hospitals. however, federal law dictates that an individual has the right to access his or her medical records. Dec 09, 2020 · medical software tools with built-in soap notes templates. if you’re willing to invest, there are specific medical software systems that offer built-in templates. with built-in soap notes, all patient records you enter are directly linked to and saved on your medical software. we’ve listed the top three software tools that have soap note.
Healthcare workers use subjective, objective, assessment, and plan (soap) notes to relay helpful and organized information about patients between professionals. soap notes get passed along to multiple people, so be clear and concise while you write them. • the “soap” note o s = subjective (what the patient tells you) o o = objective (info from pe, labs, radiology) o a = assessment (dx and ddx) o p = plan (treatment, further tests, etc. ) • discharge summary o narrative in format o summarizes the events of a hospital stay o subjective terminology is used.